Understanding RPNI and Its Impact
After an amputation, the severed nerves in the residual limb remain active. Without a target, these nerves can form painful neuromas—bundles of nerve endings that cause discomfort, phantom limb sensations, and difficulty using prosthetics.
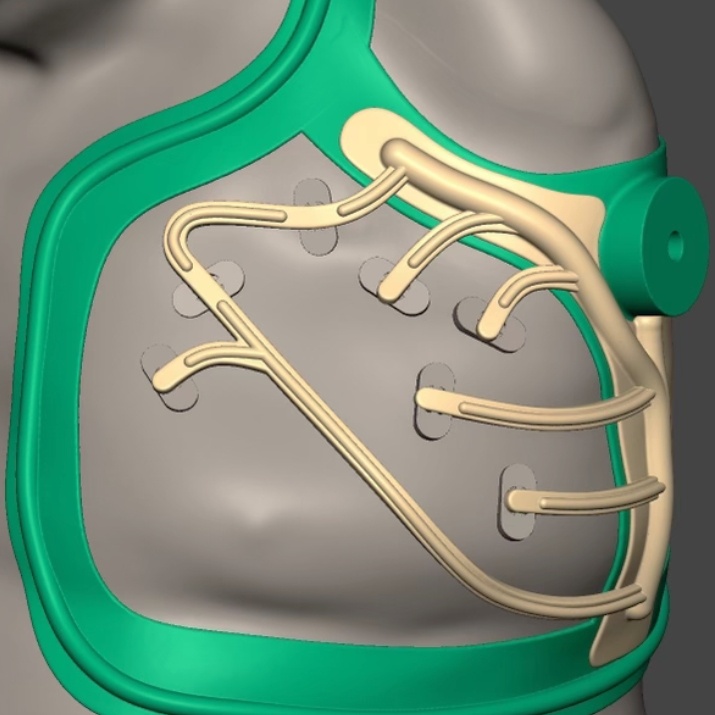
How RPNI Works
Step 1: Identifying Residual Nerves
Our surgeons locate severed nerves that may be causing pain or limiting mobility.
Step 2: Implanting Muscle Grafts
Using advanced microsurgical techniques, surgeons place each nerve end into a small muscle graft, allowing the nerve fibers to regenerate naturally.
Step 3: Enhancing Recovery & Prosthetic Control
The muscle grafts act as bioelectrical amplifiers, improving nerve signal clarity for myoelectric prosthetics and reducing pain.
Is RPNI Right for You?
RPNI can be life-changing for many patients with amputations. Our team works with you to decide whether the nerve interface procedure aligns with your recovery goals. It may be a good option if you are experiencing:
Neuroma-related pain in your residual limb
Phantom limb pain that has not responded to other treatments
Limited control of a myoelectric prosthesis
What to Expect With RPNI Surgery

Before Surgery
RPNI can be performed as part of an initial amputation procedure or as a separate surgery. Each patient's needs may differ based on their medical situation, and our specialists will help determine the most appropriate timing for the procedure.
%20(T3)%20-%20During%20Surgery.jpg?width=715&height=484&name=ARMS%20-%20Regenerative%20Peripheral%20Nerve%20Interface%20(RPNI)%20(T3)%20-%20During%20Surgery.jpg)
During Surgery
Your surgeon will carefully implant the severed nerves into muscle grafts using precise microsurgical techniques. These grafts provide a biologically active environment that encourages proper nerve regeneration. By integrating with surrounding tissues, the muscle grafts help redirect nerve growth, reducing the risk of abnormal nerve activity and improving functional outcomes.

After Surgery
Most patients stay in the hospital for 1–2 nights following surgery for monitoring and recovery. During this time, our team will:
- Monitor circulation, nerve function, and overall healing
- Provide post-surgical pain management and care instructions
- Help you prepare for the next steps in prosthetic fitting and rehabilitation
Our team is dedicated to ensuring you’re as comfortable as possible and well-prepared for the next stage of your recovery.
%20(T3)%20-%20step%20toward%20reliefe.jpg?width=611&height=611&name=ARMS%20-%20Regenerative%20Peripheral%20Nerve%20Interface%20(RPNI)%20(T3)%20-%20step%20toward%20reliefe.jpg)
How RPNI Works With TMR
RPNI and Targeted Muscle Reinnervation (TMR) are often used together for optimal pain relief and prosthetic control.
- TMR redirects severed nerves to the nerves that control larger functional muscles, reducing pain and improving prosthetic control.
- RPNI provides muscle grafts for nerves without available muscle targets, preventing neuroma formation.
- Combined, these techniques maximize nerve integration and prosthetic signal clarity.
Why Choose ARMS for RPNI?
Our team combines advanced expertise in RPNI with a deep commitment to your recovery, guiding you toward relief and renewed confidence.
Expertise in Microsurgical Procedures
Comprehensive Care Under One Roof
Personalized Treatment Plans
We take the time to understand your pain, challenges, and goals, delivering empathetic and effective care.
Take the First Step Toward Relief
If pain or prosthetic challenges are affecting your quality of life, a nerve interface procedure like RPNI may be the solution you need. Our team at ARMS is here to guide you every step of the way.
Frequently Asked Questions About RPNI
Unlike traditional nerve surgery or medication-based treatments, RPNI offers a long-term solution by integrating nerves with muscle grafts, reducing neuroma formation and enhancing prosthetic control.
Yes, RPNI can be combined with TMR or other reconstructive procedures to optimize pain relief and prosthetic function. Our team will determine the best approach based on your needs.
Rehabilitation typically includes physical therapy to strengthen surrounding muscles, optimize prosthetic function, and ensure proper nerve healing. Our team will provide a customized recovery plan.
As with any surgical procedure, risks may include infection, swelling, or delayed healing. However, our specialized team uses advanced techniques to minimize complications and support a smooth recovery.
RPNI can be performed at the time of amputation or later, depending on your condition. Your surgeon will discuss the best timing based on your recovery goals.